Restoring Vision: The Science of Retinal Implants
In a world defined by sight, the loss of this precious sense can be a profoundly isolating experience. For millions suffering from degenerative retinal diseases like retinitis pigmentosa and age-related macular degeneration, the world slowly fades into a blur, and then into darkness. But in the labs and operating rooms at the forefront of medical innovation, a beacon of hope has emerged: the retinal implant. This marvel of biomedical engineering, often dubbed the "bionic eye," represents a new frontier in restoring a semblance of sight to the blind. This comprehensive exploration delves into the intricate science behind retinal implants, tracing their historical evolution, dissecting the technology, and sharing the poignant stories of those who have embarked on this remarkable journey to reclaim a part of their visual world.
A Glimmer of Hope: The Genesis of Artificial Vision
The concept of using electricity to evoke a sensation of sight is not a new one. As far back as the 18th century, scientists and thinkers, including the likes of Benjamin Franklin, were intrigued by the idea of stimulating the visual system with electrical currents. The first documented attempt to use electricity for vision restoration dates back to 1755, when French physician Charles Le Roy applied an electrical current to the eye of a blind patient, who reported seeing flashes of light, or "phosphenes." This rudimentary experiment, though unsuccessful in restoring functional vision, planted a seed that would take centuries to fully germinate.
The 20th century witnessed more systematic investigations into the electrical stimulation of the visual cortex, the part of the brain that processes visual information. In 1929, German neurosurgeon Otfrid Foerster demonstrated that stimulating the occipital lobe could reliably produce phosphenes in a patient's visual field. This discovery was a crucial step, confirming that the brain's visual centers could be artificially activated.
The mid-20th century saw the first tangible steps towards a true visual prosthesis. In 1956, Graham Tassicker, an Australian engineer, implanted a light-sensitive selenium cell behind the retina of a blind volunteer, who transiently regained the ability to perceive light. This was a landmark achievement, marking the first time a device was implanted to directly interact with the retina.
A pivotal moment in the history of retinal implants came in 1968, when Drs. Giles Brindley and W.S. Lewin developed and implanted a device that stimulated the visual cortex. Their work demonstrated the feasibility of creating visual percepts using direct electrical stimulation and spurred further research into implantable devices for vision restoration.
The latter half of the 20th century saw a surge in research and development, fueled by advancements in microelectronics and surgical techniques. Pioneers like William H. Dobelle continued to refine cortical implants, creating the "Dobelle eye" in the 1980s and 90s. However, these early cortical implants presented significant surgical challenges and often resulted in complications.
The focus then shifted towards the retina, a more accessible and, in some ways, more logical target for stimulation. In patients with diseases like retinitis pigmentosa and age-related macular degeneration, the light-sensing photoreceptor cells are lost, but the inner retinal neurons that transmit signals to the brain often remain relatively intact. This realization was a turning point, leading to the development of retinal prostheses designed to bypass the damaged photoreceptors and directly stimulate these surviving neurons.
The late 20th and early 21st centuries saw the emergence of several research groups and companies dedicated to developing retinal implants. The first Argus I device, a 16-electrode epiretinal implant, was implanted in 2002. This was followed by the Argus II, a more advanced 60-electrode system, which received CE mark approval in Europe in 2011 and FDA approval in the United States in 2013, becoming the first commercially available retinal implant. Around the same time, the Alpha-IMS, a subretinal implant developed by Retina Implant AG in Germany, also received CE mark approval. These milestones marked the dawn of a new era in the treatment of blindness, transforming a once-futuristic concept into a clinical reality.
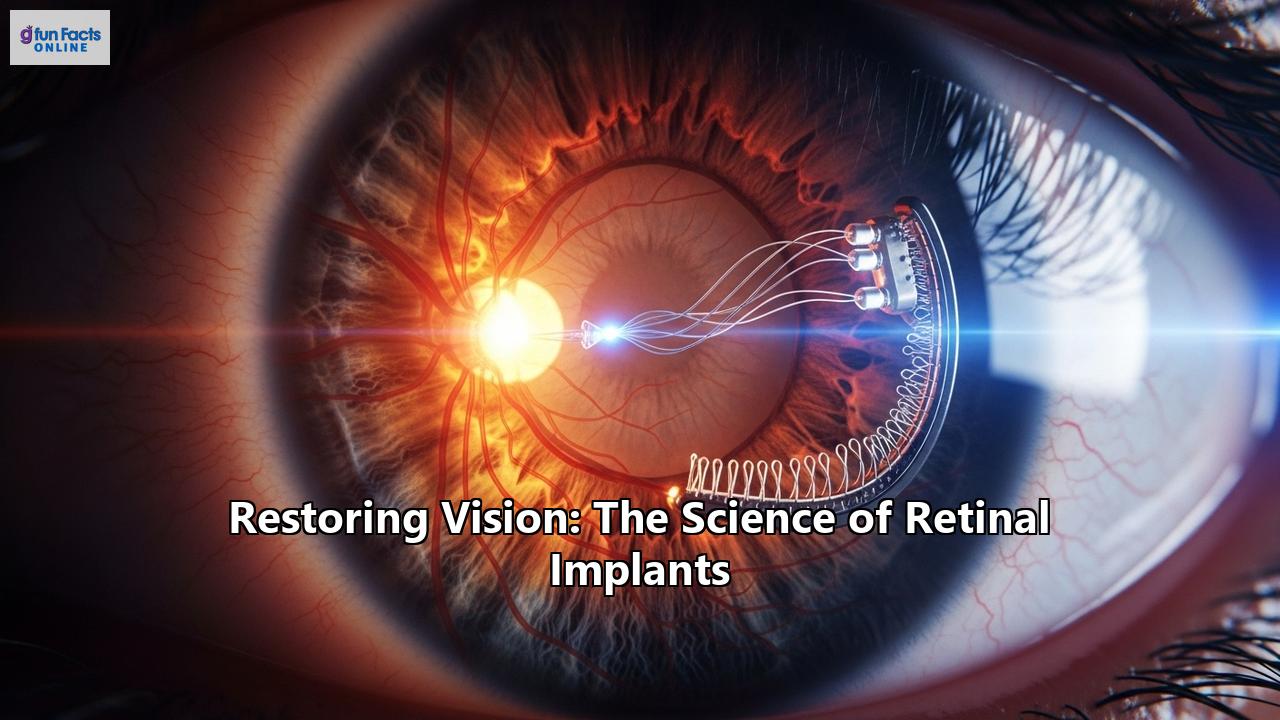
The Inner Workings: How Retinal Implants Create a New Kind of Sight
Retinal implants, at their core, are sophisticated electronic devices that translate light into electrical signals that the brain can interpret as vision. They are designed to replace the function of the damaged or missing photoreceptor cells in the retina. The fundamental principle involves electrically stimulating the remaining healthy retinal neurons, which then send these artificial signals to the brain via the optic nerve. The brain, in turn, learns to interpret these patterns of electrical stimulation as spots of light, or phosphenes, which can be pieced together to form a rudimentary image.
While the overarching principle is the same, different types of retinal implants employ distinct strategies to achieve this goal. These can be broadly categorized based on their placement within the eye: epiretinal, subretinal, and suprachoroidal.
Epiretinal Implants: On the Surface of the Retina
Epiretinal implants are placed on the inner surface of the retina, directly stimulating the retinal ganglion cells, the final output neurons of the retina that send signals to the brain. This approach has the advantage of a relatively less complex surgical procedure, as the implant is placed on top of the retina rather than within its delicate layers.
The most well-known example of an epiretinal implant is the Argus II Retinal Prosthesis System. This system consists of both external and internal components. The external part includes a small video camera mounted on a pair of glasses, which captures images from the environment. These images are then sent to a small, wearable video processing unit (VPU) that converts them into a simplified electrical signal. This signal is transmitted wirelessly to the internal implant, which consists of a receiving coil and an array of 60 electrodes that are tacked onto the surface of the retina. The electrodes then stimulate the ganglion cells, creating the perception of light.
Advantages of Epiretinal Implants:- Simpler surgical placement: The surgery is generally less complex and more familiar to vitreoretinal surgeons compared to subretinal implantation.
- Direct stimulation of ganglion cells: This bypasses all other retinal layers, which can be beneficial if there is damage beyond the photoreceptors.
- Good heat dissipation: The implant's interface with the vitreous cavity allows for effective heat dispersion.
- Axonal stimulation: Because the implant stimulates the ganglion cell axons that run along the surface of the retina, it can create distorted or elongated phosphenes.
- Requires an external camera: Patients need to learn to scan their environment by moving their heads rather than their eyes, as the camera's field of view is fixed relative to the head.
- Limited resolution: The number of electrodes in current devices is relatively low, resulting in a low-resolution image.
Other examples of epiretinal implants include the IRIS II by Pixium Vision and the EPI-RET 3.
Subretinal Implants: Beneath the Retina's Surface
Subretinal implants are placed in the subretinal space, between the photoreceptor layer and the retinal pigment epithelium (RPE). This location is anatomically closer to the natural position of the photoreceptors, and the implants are designed to stimulate the bipolar cells, which are the next layer of neurons in the visual pathway.
A prominent example of a subretinal implant is the Alpha-AMS, developed by Retina Implant AG. This device features a microchip with 1600 photodiodes that is implanted under the retina. Unlike the Argus II, the Alpha-AMS does not require an external camera. Instead, the photodiodes on the chip itself detect the light that enters the eye naturally. The chip then converts this light into electrical signals that stimulate the overlying retinal cells. This approach allows for more natural eye movements to scan the environment.
Another innovative subretinal implant is the PRIMA system, developed by Pixium Vision. This photovoltaic implant is powered by near-infrared light projected from a pair of augmented reality glasses. The implant, which is a tiny, wireless 2x2 mm chip, converts this light into electrical signals that stimulate the inner retinal neurons.
Advantages of Subretinal Implants:- More natural vision: By utilizing the eye's natural optics and allowing for normal eye movements, subretinal implants can provide a more intuitive visual experience.
- Higher potential resolution: These implants can accommodate a larger number of electrodes, which could theoretically lead to sharper images. The Alpha-AMS, for instance, has 1600 photodiodes.
- Stimulation of bipolar cells: This approach leverages the remaining processing capabilities of the inner retina, which may result in a more coordinated and natural visual signal being sent to the brain.
- More complex surgery: The surgical procedure to place the implant in the delicate subretinal space is technically challenging and demanding for surgeons.
- Dependence on healthy inner retinal layers: The effectiveness of subretinal implants relies on the integrity of the bipolar cell layer.
- Potential for heat dissipation issues: The enclosed nature of the subretinal space can make heat dissipation from the implant more challenging.
Suprachoroidal Implants: A Less Invasive Approach
Suprachoroidal implants are placed in the suprachoroidal space, between the choroid (a layer of blood vessels) and the sclera (the white of the eye). This is a less invasive surgical approach as it avoids entering the vitreous cavity or manipulating the retina directly.
The Bionic Vision Australia (BVA) group and the Phoenix99 are examples of suprachoroidal devices. The BVA's second-generation device has a 44-channel electrode array, while the Phoenix99 has 98 stimulating electrodes. These devices are surgically placed in the suprachoroidal space and are coupled with an external camera system, similar to epiretinal implants.
Advantages of Suprachoroidal Implants:- Less invasive surgery: The surgical procedure is generally simpler and safer, with a lower risk of retinal detachment or damage to the lens.
- Stable implant position: The suprachoroidal space provides a secure location for the implant.
- Wider field of view: This approach allows for the placement of larger electrode arrays, which can provide a wider field of vision, beneficial for navigation and orientation.
- Higher stimulation threshold: Due to the increased distance from the retinal neurons, suprachoroidal implants require more electrical power to elicit a visual response.
- Risk of hemorrhage: The choroid is a highly vascularized tissue, so there is a significant risk of bleeding during surgery.
- Limited resolution: The distance from the retina may limit the potential for high-acuity vision.
The Surgical Odyssey: Implanting a Bionic Eye
The journey to receiving a retinal implant culminates in a complex and delicate surgical procedure that requires the expertise of a highly skilled vitreoretinal surgeon. The specifics of the surgery vary depending on the type of implant being placed, but all procedures are performed under general anesthesia and can take several hours to complete.
Epiretinal Implant Surgery
The implantation of an epiretinal device like the Argus II involves a combination of standard and novel surgical techniques. The procedure typically begins with a vitrectomy, where the vitreous gel that fills the eye is removed to provide access to the retina. The surgeon may also need to remove any scar tissue or membranes from the surface of the retina where the implant will be placed.
The implant itself, which consists of the electrode array and a small electronics package, is then carefully inserted into the eye. The electronics package is secured to the outside of the eye, similar to a scleral buckle used for retinal detachment surgery. The delicate electrode array is then placed on the surface of the macula, the central part of the retina responsible for detailed vision, and is held in place with a tiny retinal tack.
Subretinal Implant Surgery
The surgical placement of a subretinal implant, such as the Alpha-AMS or PRIMA, is a more intricate and technically demanding procedure. The surgery also begins with a vitrectomy. Then, the surgeon creates a small, controlled retinal detachment by injecting fluid under the retina, creating a space for the implant.
For a device like the Alpha-AMS, a transchoroidal approach is used to pass a polyimide foil carrying power and signals to the implant. The implant chip is then carefully guided into the subretinal space through a small incision in the retina. The precise positioning of the chip under the fovea, the center of the macula, is crucial for achieving the best possible visual outcome and is one of the most challenging aspects of the surgery. Once the implant is in place, the retina is reattached.
The PRIMA implant surgery involves a similar process of creating a subretinal bleb and then inserting the tiny 2mm chip into this space.
Suprachoroidal Implant Surgery
The surgical procedure for a suprachoroidal implant is considered less invasive than the other two approaches. The surgeon creates an incision in the sclera and then carefully dissects a pocket in the suprachoroidal space. The electrode array is then inserted into this pocket and positioned beneath the macula. The external components, such as the receiver coil, are secured to the outside of the eye. This approach avoids the need for a vitrectomy and direct manipulation of the retina, reducing the risk of certain complications.
A New World of Sight: Patient Experiences and Rehabilitation
Receiving a retinal implant is not a simple fix that instantly restores natural vision. Instead, it marks the beginning of a long and often arduous journey of learning to see in a completely new way. The vision provided by these devices is not a high-resolution, full-color picture of the world, but rather a series of light flashes, or phosphenes, that the brain must learn to interpret.
The "Switch-On" Moment and the Nature of Artificial Vision
One of the most profound moments for a retinal implant recipient is the initial activation of the device, often referred to as the "switch-on." For many who have lived in darkness for years, the perception of light, even just a single point, can be an intensely emotional experience. Larry Hester, one of the first patients in the US to receive the Argus II, described the moment his implant was turned on: "It was incredible. It was bright. And it was significant...it was hard to articulate what I was feeling but I wanted to share it with everybody I could grab at the time and hug."
Patients consistently describe the visual percepts from their implants as being fundamentally different from natural vision. They often use terms related to electricity, such as "flashes," "sparks," or "twinkles," to describe what they "see." This artificial vision is a learned skill, requiring the recipient to build a "lexicon of flashes" – a new perceptual vocabulary to understand their surroundings.
The Long Road of Rehabilitation
After the implant is activated, patients undergo a rigorous and intensive rehabilitation program to learn how to use their new sense of sight. This training is crucial for maximizing the functional benefits of the implant and can last for several months.
The rehabilitation process is multifaceted and tailored to the individual needs of the patient. It often includes:
- Basic Task Training: Patients start with simple tasks like detecting a light source, distinguishing between light and dark, and identifying basic shapes.
- Scanning Techniques: For implants that use an external camera, patients must learn to scan their environment by moving their head to build a mental picture of their surroundings.
- Object Recognition: As they become more proficient, patients practice identifying and locating everyday objects.
- Orientation and Mobility: A significant part of the training focuses on using the implant to navigate, such as following a line on the floor, finding a doorway, or avoiding obstacles.
- Eye-Hand Coordination: Specific exercises are designed to improve the ability to reach for and grasp objects.
With dedicated training, some patients have achieved remarkable results, including reading large-print words, recognizing faces, and even participating in activities like skiing or mountain climbing. One Argus II recipient shared how he could see fireworks for the first time in 25 years, a "wonderful" and "uplifting" experience. Another patient, Sheila Irvine, who received the PRIMA implant, spoke of her excitement at being able to see letters again and the joy of rediscovering her love for reading.
The Challenges of Living with a Bionic Eye
Despite the incredible potential of retinal implants, living with one is not without its challenges. The vision provided is often described as "blurry" or "pixelated," and it requires a significant amount of cognitive effort to interpret the signals. Many patients report that using the device is mentally taxing and can only be done for limited periods.
Managing expectations is another critical aspect of the patient journey. While the technology is life-changing for some, it does not restore natural sight, and the outcomes can vary widely between individuals. The emotional toll of this process can be significant, and some patients may even experience a renewed sense of grief over their vision loss.
Furthermore, the long-term reliability and support for these devices are major concerns. The case of Second Sight, the manufacturer of the Argus II, which discontinued the device and left patients without support for repairs or maintenance, highlights the vulnerability of recipients who depend on this technology. This has raised important ethical questions about the responsibilities of medical device companies to their patients.
The Horizon of Vision Restoration: Future Developments
The field of retinal implants is in a constant state of evolution, with researchers around the world working to overcome the limitations of current devices and develop new and more effective ways to restore sight.
Smaller Pixels, Higher Resolution
A key area of focus is on increasing the number of electrodes in the implants to improve the resolution of the artificial vision. The goal is to move from the "blobby," impressionistic images of current devices to a more detailed, "pointillist" view of the world. Researchers are also working on developing smaller and more efficient electrodes that can be placed closer to the retinal neurons, allowing for more precise stimulation with less power.
The Rise of Optogenetics
One of the most exciting and potentially transformative areas of research is optogenetics. This cutting-edge technique involves using gene therapy to introduce light-sensitive proteins into the remaining retinal cells, making them responsive to light. This could, in theory, allow for much more precise and naturalistic stimulation of the retina than is possible with electrical implants. While still in the early stages of research, optogenetics holds the promise of a biological solution to vision restoration.
Bypassing the Eye: Cortical and Optic Nerve Implants
For individuals whose blindness is caused by damage to the optic nerve or who have no eyes at all, retinal implants are not an option. For these patients, researchers are developing cortical implants that bypass the eye and optic nerve entirely, stimulating the visual cortex of the brain directly. While early cortical implants had limited success, newer devices with more advanced technology are showing promise in clinical trials.
Another approach is the development of optic nerve implants, which aim to stimulate the optic nerve directly. These devices could be a viable option for patients with a healthy optic nerve but a severely damaged retina.
The "Smart" Bionic Eye
The integration of artificial intelligence (AI) is poised to revolutionize retinal implant technology. The concept of a "smart" bionic eye involves using AI-powered image processing to enhance the visual information sent to the implant. For example, AI could be used to highlight important objects in the environment, such as faces or obstacles, or to provide real-time audio cues to the user. This could make the artificial vision more practical and useful for everyday tasks.
The Ethical Landscape: Navigating the Complexities of a New Technology
As with any groundbreaking medical technology, retinal implants raise a host of complex ethical questions. The high cost of these devices, which can be upwards of $100,000, raises concerns about accessibility and equity. Who gets to benefit from this life-changing technology, and how do we ensure that it is not just available to the wealthy?
The long-term health implications and the durability of the implants are also significant considerations. As the case of Second Sight demonstrated, patients can be left in a difficult position if the company that manufactured their implant goes out of business. This highlights the need for robust regulatory oversight and long-term support systems for patients.
Informed consent and the management of patient expectations are also critical ethical issues. It is essential that patients have a clear understanding of the limitations of the technology and the commitment required for rehabilitation. The decision to undergo such a life-altering procedure should be made with full awareness of both the potential benefits and the significant challenges.
A Future in Sight
The science of retinal implants has come a long way from the early experiments with electrical stimulation. Today, a handful of devices have been successfully implanted in hundreds of patients, offering them a renewed sense of connection to the world. While the vision they provide is still a far cry from natural sight, for those who have lived in darkness, even the ability to see the outline of a loved one's face or the twinkling of Christmas lights can be a profoundly moving and life-affirming experience.
The journey to restore sight is far from over. The path forward is paved with both immense promise and significant challenges. But with each new discovery, each refinement in technology, and each courageous patient who embarks on this journey, we move one step closer to a future where blindness is no longer an insurmountable barrier, a future where the world, in all its vibrant detail, can be seen once more.
Reference:
- https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0229189
- https://www.youtube.com/watch?v=4gWjp7yAoII
- https://pmc.ncbi.nlm.nih.gov/articles/PMC12496445/
- https://www.fightingblindness.ca/resources/the-bionic-eye/
- https://www.ophthalmologytimes.com/view/testimonial-argus-ii-retinal-prosthesis-system-video
- https://www.youtube.com/watch?v=8AWIJdayKow
- https://www.youtube.com/watch?v=2-BsV0sYetk
- https://www.moorfields.nhs.uk/about-us/news-and-blogs/news/pioneering-eye-device-restores-reading-vision-to-blind-eyes
- https://www.retina-specialist.com/article/reallife-story-of-the-bionic-eye-the-argus-iia
- https://www.researchgate.net/publication/360702990_Visual_Rehabilitation_after_Retinal_Prosthesis_Implantation_An_18-month_Case_Report_From_Candidate_Selection_to_Follow-Up
- https://iovs.arvojournals.org/article.aspx?articleid=2692175
- https://www.retinalphysician.com/issues/2024/may/overview-of-retinal-prosthesis-and-future-directions/
- https://dkeyecarehospital.com/artificial-retina-implant-eye-hospital/
- https://www.youtube.com/watch?v=CiyGOUHD2nI
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7875418/
- https://www.youtube.com/watch?v=UnrLaDCTOwA
- https://www.macularsociety.org/about/media/news/2025/october/revolutionary-implant-allows-patients-with-dry-amd-to-read-again/
- https://www.aao.org/eyenet/article/retinal-prostheses-progress-problems
- https://bionicvisionlab.org/research/smart-bionic-eye/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3787184/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7198351/